Around the globe, an estimated 1.2 million stillbirths occur after the onset of labor and 1 million live-born infants die on their birth day, indicating the increased importance of high-quality care during the time of birth. In Nepal, 36% of neonatal deaths are due to intrapartum-related complications and 23% of stillbirths occur during the intrapartum period. Many interventions have been discovered and implemented to upgrade quality of care. Resuscitation at the right time following evidence based guideline by trained personnel have an outstanding effect in lowering about 30% of the neonatal deaths. A basic neonatal resuscitation protocol called Helping Babies Breathe (HBB) has been developed for use in low-resource settings. It was designed to improve health workers’ awareness of the need to initiate neonatal resuscitation within the first one minute, also called “Golden Minute,” to improve their clinical skills, and to increase adherence to neonatal resuscitation protocol. With the aim to improve adherence to the Helping Babies Breathe (HBB) neonatal resuscitation protocol and reduce perinatal mortality by using a quality improvement cycle (QIC) a clinical trial was conducted in a tertiary hospital in Nepal in collaboration with Uppsala University, Sweden.

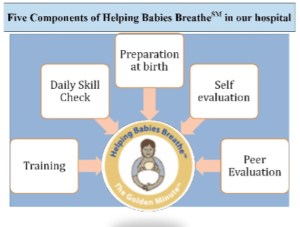
In 2012, in a tertiary hospital, Paropakar Maternity Hospital, there were ∼22 000 deliveries at the hospital, with a stillbirth rate of 19 per 1000 deliveries and an early neonatal mortality rate of 9 per 1000 live births. The HBB QIC was implemented through a multifaceted approach, including the formation of quality improvement teams; development of quality improvement goals, objectives, and standards; HBB protocol training; weekly review meetings; daily skill checks; use of self-evaluation checklists; and refresher training.
A cohort design, including a nested case-control study was used to measure changes in clinical outcomes and adherence to the resuscitation protocol through video recording, before and after implementation of the QIC. The intrapartum stillbirth rate decreased from 9.0 to 3.2 per thousand deliveries, and first-day mortality from 5.2 to 1.9 per thousand live births after intervention, demonstrating a reduction of approximately half in the odds of intrapartum stillbirth (adjusted odds ratio [OR] 0.46, 95% confidence interval [CI] 0.32–0.66) and first-day mortality (adjusted OR 0.51, 95% CI 0.31–0.83). After intervention, the odds of inappropriate use of suction and stimulation decreased by 87% (OR 0.13, 95% CI 0.09–0.17) and 62% (OR 0.38, 95% CI 0.29–0.49), respectively. Before intervention, none of the infants received bag-and-mask ventilation within 1 minute of birth, compared with 83.9% of infants after.

Eventually, stillbirths were reduced using a standard resuscitation protocol by trained human resources actively participating in QIC. Proper suctioning and stimulation were now the improved clinical practices at birth. The consequences directed towards the scale up of the trial across Nepal to achieve quality care and ultimately healthy newborns.



